

Similar to what was previously shown ( 3, 20), COVID-19 vaccination induced robust S1 or RBD-specific plasma IgG at levels comparable to severe cases of natural infection ( Fig. We first performed enzyme-linked immunoassay (ELISA) to determine and compare the SARS-CoV-2 S1 or receptor binding domain (RBD)-specific IgG, IgA and IgM levels in unvaccinated control (non-SARS-CoV-2 infected), vaccinated, and convalescent groups in the plasma. We compared the vaccine-induced respiratory and circulating antibodies, as well as cellular immune responses, to those of hospitalized COVID-19 convalescent patients that we have previously recruited between September 2020 to April 2021 when the D614G and Alpha variants dominated ( 19). The vaccine type, timing of collection, age, and sex information are included in Table. Most of these individuals had received two doses of mRNA vaccination, with 3 individuals receiving the third booster and one having the J&J vaccine.

To determine the humoral and cellular immune responses following COVID-19 vaccination, we collected blood and BAL samples from 19 COVID-19-vaccinated individuals ( Fig. It is currently unclear whether efficient mucosal neutralizing antibody responses can be induced by vaccination, and/or natural infection, and to what extent this could protect against SARS-CoV-2 infection. Additionally, the SARS-CoV-2 Omicron sublineage, easily escapes both vaccine and infection-elicited antibody neutralization in the blood ( 8– 14).

Thus, we reasoned that it was critical to characterize respiratory mucosal humoral and cellular immunity following COVID-19 mRNA vaccination or natural infection to better understand the vaccine- or infection-mediated protection against SARS-CoV-2 infection. As the result, respiratory mucosal antibodies, tissue-resident memory T (T RM) and B cells are likely among the early responders during viral entry, and so they are believed to be essential for the protection against the establishment of viral infection after vaccination or prior viral exposure ( 7). However, SARS-CoV-2 enters the host predominantly through the respiratory tract. Notably, most of the previous studies were conducted using blood to determine circulating antibodies and B and T cell immunity following vaccination ( 6). Hence, mucosal booster vaccination is needed to establish robust sterilizing immunity in the respiratory tract against SARS-CoV-2, including infection by Omicron sublineage and future VOCs. Together, our study supports the contention that the current COVID-19 vaccines are highly effective against severe disease development, likely through recruiting circulating B and T cell responses during re-infection, but offer limited protection against breakthrough infection, especially by Omicron sublineage.
3D COAT ALPHAS PLUS
Using a mouse immunization model, we demonstrated that systemic mRNA vaccination alone induced weak respiratory mucosal neutralizing antibody responses, especially against SARS-CoV-2 Omicron BA.1.1 in mice however, a combination of systemic mRNA vaccination plus mucosal adenovirus-S immunization induced strong neutralizing antibody responses, not only against the ancestral virus but also the Omicron BA.1.1 variant. Furthermore, mRNA vaccination induced circulating S-specific B and T cell immunity, but in contrast to COVID-19 convalescents, these responses were absent in the BAL of vaccinated individuals. Vaccinated individuals had significantly lower levels of neutralizing antibody against D614G, Delta (B.1.617.2) and Omicron BA.1.1 in the BAL compared to COVID-19 convalescents, despite robust S-specific antibody responses in the blood. We compared the SARS-CoV-2 S-specific total and neutralizing antibody responses, and B and T cell immunity, in the bronchoalveolar lavage fluid (BAL) and blood of COVID-19 vaccinated individuals and hospitalized patients. SARS-CoV-2 mRNA vaccination induces robust humoral and cellular immunity in the circulation however, it is currently unknown whether it elicits effective immune responses in the respiratory tract, particularly against variants of concern (VOCs), including Omicron.
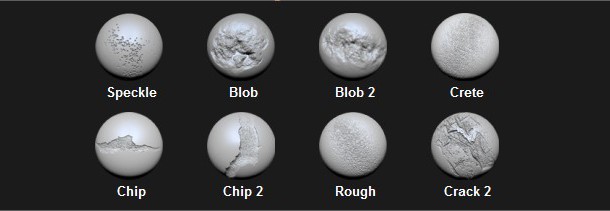
Kaplan, Drew Weissman, Ryan Kern, Haitao Hu, Robert Vassallo, Shan-Lu Liu, and Jie Sun Show Fewer Cox, Chaofan Li, Young Min Son, In Su Cheon, Yue Wu, … Show All …, Supriya Behl, Justin J. 3DCoat is the one application that has all the tools you need to take your 3D idea from a block of digital clay all the way to a production ready, fully textured organic or hard surface model.Jinyi Tang, Cong Zeng, Thomas M.


 0 kommentar(er)
0 kommentar(er)
